A risk-based approach to regulatory actions is adopted. The risk level of non-compliance is assessed by how likely it would impact on patient safety (Table 1) and the seriousness of consequence in terms of patient harm that the non-compliance could cause (Table 2). The likelihood of impact on patient safety and consequence level are cross-matched against the risk matrix (Table 3) to guide the decision-making process on the regulatory actions to be undertaken.
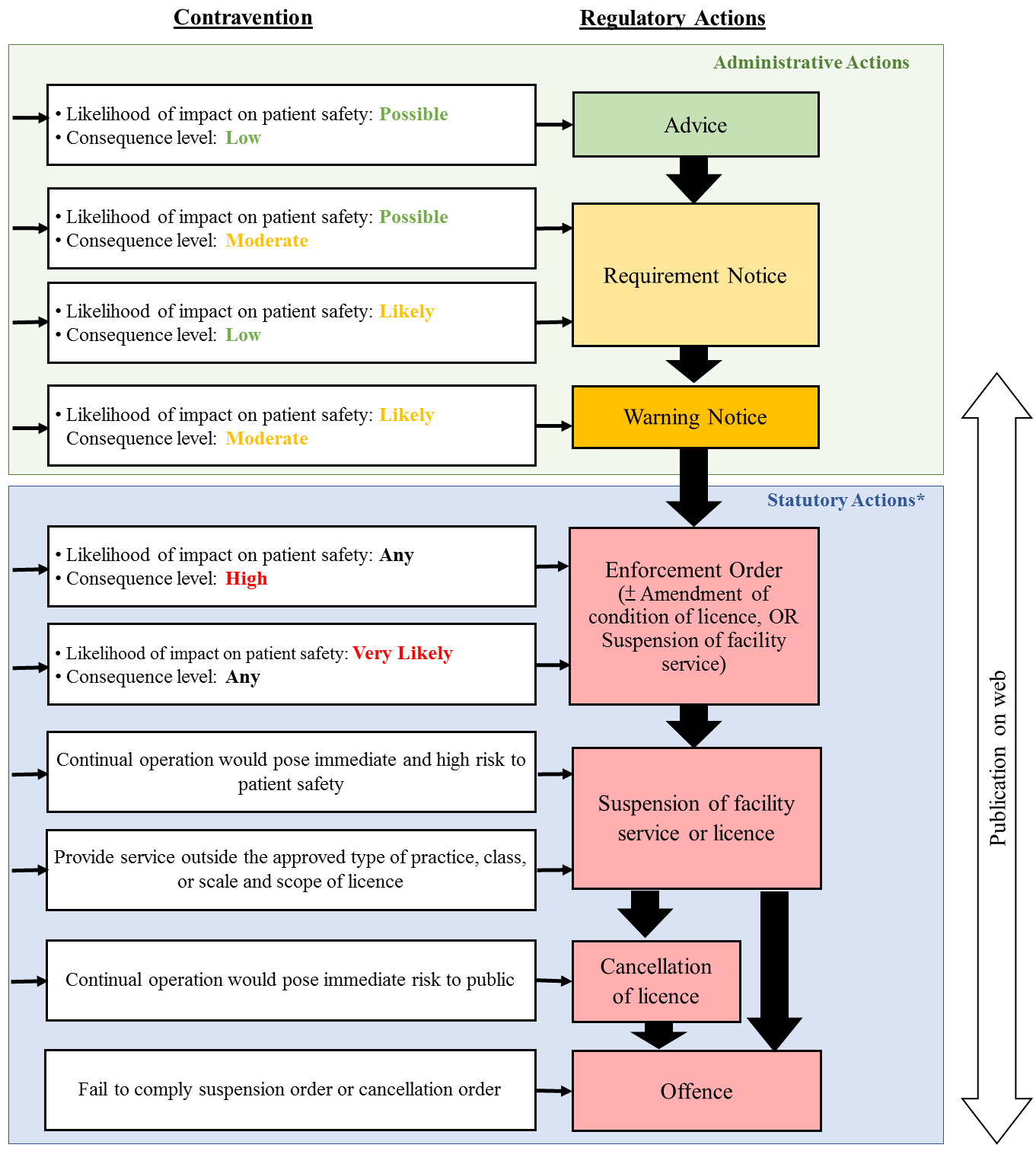
Depending on the risk level involved, regulatory actions against non-compliances may include (a) advice, (b) requirement notice, (c) warning notice, (d) enforcement order, (e) amendment of condition of licence, (f) suspension of facility service or licence, and (g) cancellation of licence. Records on regulatory actions may be published on the website of the Office for Regulation of Private Healthcare Facilities for public reference. Details of the regulatory actions according to the risk level of contravention are set out in Figure 1 & Figure 2.
PHFs are expected to take immediate actions to rectify non-compliances to mitigate risks to patient safety. If a PHF does not rectify the non-compliance within the timeframe imposed or the rectification is unsatisfactory, regulatory actions may be escalated in accordance with the risk level.
On the other hand, stronger regulatory actions could also be imposed in accordance with the level of risk which the PHF had involved, without going through a staged approach as mentioned above. For instance, if it is considered that continual operation of a PHF would pose immediate and high risk to patient safety, the PHF concerned would be requested to suspend the facility service with no prior warning required.
| Likelihood of impact on patient safety | Description |
| Possible | Consequence for patient safety may arise, if no appropriate actions were taken by the PHF |
| Likely | Consequence for patient safety will probably happen, if no appropriate actions were taken by the PHF |
| Very likely | Consequence for patient safety is expected to arise, if no appropriate actions were taken by the PHF |
| Level | Patient harm |
| Low | Negligible or minor patient harm |
| Moderate |
There was patient harm as defined by the following conditions:
|
| An event which impacts on more than one but less than five patients | |
| High |
There was patient harm as defined by the following conditions:
|
| An event which impacts on five or more patients |
| Consequence level of non-compliance | |||
| Likelihood of impact on patient safety | Low | Moderate | High |
| Possible | Advice | Requirement Notice | Enforcement Order ±Amend / Suspend* |
| Likely | Requirement Notice | Warning Notice | Enforcement Order ±Amend / Suspend* |
| Very likely | Enforcement Order ±Amend / Suspend* |
Enforcement Order ±Amend / Suspend* |
Enforcement Order ±Amend / Suspend* |
 * Pursuant to section 37(1), 29 and 28(b) of the Private Healthcare Facilities Ordinance, the Director of Health may amend the condition of a licence for, suspend a facility service in, or by order suspend or cancel a licence a private healthcare facility on a ground specified in section 38.
* Pursuant to section 37(1), 29 and 28(b) of the Private Healthcare Facilities Ordinance, the Director of Health may amend the condition of a licence for, suspend a facility service in, or by order suspend or cancel a licence a private healthcare facility on a ground specified in section 38.
Note:
- Directions by Notice may be given when immediate direction is required on remedial action(s) to be taken by PHF.
 Escalation of regulatory action take place when:
Escalation of regulatory action take place when:
- Non-compliance not rectified within the time frame imposed or rectification is unsatisfactory; OR
- No satisfactory remedial action after two pieces of Advice or Requirement Notices issued within the past 12 months (related or unrelated non-compliances)

